Spirometry: the #1 tool in successful asthma management
This article has been reviewed by Elina Kiviaho
Introduction
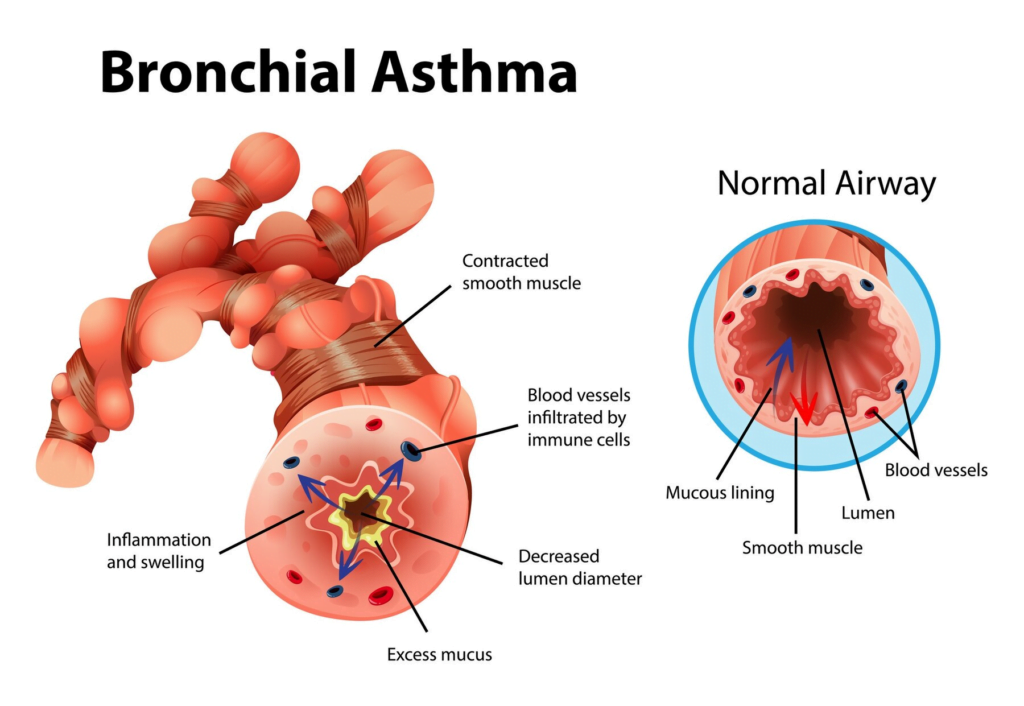
Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways, leading to episodes of wheezing, breathlessness, chest tightness, and coughing. These symptoms can vary in frequency and severity, significantly impacting the quality of life for millions of individuals worldwide. Effective management of asthma is essential to control symptoms, prevent exacerbations, and maintain optimal lung function.
Spirometry is a fundamental diagnostic and monitoring tool in the management of asthma. This simple, non-invasive test measures how much air a person can exhale and how quickly they can do so. By providing objective data on lung function, spirometry helps healthcare providers diagnose asthma accurately, monitor disease progression, and tailor treatment plans to individual patient needs.
Incorporating spirometry into routine asthma care is crucial for optimizing patient outcomes. It allows for early detection of changes in lung function, enabling timely interventions to prevent asthma attacks. This article explores the role of spirometry in asthma management, highlighting its benefits, practical applications, and future directions in respiratory healthcare.
Overview of asthma as a chronic respiratory condition
Asthma is a complex, heterogeneous disease characterized by chronic inflammation of the airways. This inflammation leads to hyperresponsiveness and airflow limitation, presenting as episodes of wheezing, breathlessness, chest tightness, and coughing. The prevalence of asthma varies globally, with significant morbidity and mortality associated with uncontrolled asthma. The etiology of asthma involves genetic predisposition and environmental factors, including allergens, respiratory infections, and pollutants. Effective management is crucial to control symptoms, prevent exacerbations, and improve patient outcomes (CCJM) (ERS Journals).
Brief introduction to spirometry
Spirometry is the most widely used objective test for diagnosing and monitoring respiratory diseases. It measures the volume of air a person can exhale forcefully after maximal inhalation (Forced Vital Capacity, FVC) and the volume of air exhaled in the first second of the FVC maneuver (Forced Expiratory Volume in one second, FEV1). These measurements are essential for assessing lung function, identifying airflow obstruction, and differentiating asthma from other respiratory conditions such as chronic obstructive pulmonary disease (COPD) (ERS Journals). You can read about it in more detail in our other article – Spirometry – how it works.
The role of spirometry in asthma management is multifaceted. It aids in the accurate diagnosis of asthma, monitoring disease progression, tailoring treatment plans, and predicting exacerbations. By providing objective data, spirometry enables healthcare professionals to make informed decisions, ensuring effective and personalized asthma management (CCJM) (ERS Journals).
Benefits of spirometry in asthma management
Accurate diagnosis of asthma
Asthma diagnosis relies on clinical history, physical examination, and objective tests. Spirometry is paramount in this process, confirming airflow limitation and reversibility. The hallmark of asthma on spirometry is a reduced FEV1/FVC ratio, which improves significantly after bronchodilator administration. This reversibility distinguishes asthma from fixed airflow obstruction seen in COPD, ensuring appropriate diagnosis and management (ERS Journals) (AAFP).
Monitoring asthma control and progression
Regular spirometry is crucial for monitoring asthma control and detecting changes in lung function over time. According to the Global Initiative for Asthma (GINA) guidelines, spirometry should be performed at the initial assessment, after treatment initiation and stabilization, and periodically thereafter. This helps track disease progression, assess response to therapy, and adjust treatment as needed. Spirometry identifies deterioration in lung function, prompting timely intervention to prevent exacerbations (CCJM) (AAFP).
Tailoring asthma treatment plans
Spirometry results guide the personalization of asthma treatment plans. Patients with persistent airflow limitation may require higher doses of inhaled corticosteroids or the addition of long-acting bronchodilators. Conversely, well-controlled asthma with normal spirometry results may allow for step-down therapy. This approach minimizes medication side effects while maintaining optimal asthma control. By tailoring treatment to spirometry findings, healthcare providers can enhance patient outcomes and adherence to therapy (CCJM).
Consider the case of a 35-year-old woman with a history of wheezing and shortness of breath. She underwent spirometry, which showed an FEV1 of 70% of the predicted value and an FEV1/FVC ratio of 0.65. After using a bronchodilator, her FEV1 improved to 85% of the predicted value, confirming the diagnosis of asthma with reversible airway obstruction.
Another example involves a 10-year-old boy with poorly controlled asthma despite regular medication use. Spirometry revealed significant variability in FEV1 measurements, prompting adjustments to his treatment plan. After optimizing his medication regimen and incorporating additional preventive measures, his spirometry results stabilized, reflecting better asthma control and fewer symptoms.
These practical examples highlight the essential role of spirometry in diagnosing asthma, tailoring treatment plans, and monitoring disease progression. By incorporating spirometry into routine clinical practice, healthcare providers can ensure more precise and effective management of asthma, ultimately improving patient outcomes.
Predicting asthma exacerbations
One of the critical roles of spirometry is in predicting asthma exacerbations. Reduced lung function, indicated by a decline in FEV1, often precedes clinical symptoms of an exacerbation. Regular spirometry can identify these declines early, allowing for preemptive adjustments in treatment. Studies have shown that patients with lower baseline FEV1 are at a higher risk of severe exacerbations, emphasizing the importance of routine lung function monitoring in asthma management (CCJM) (AAFP).
Challenges and Limitations of Spirometry
Factors affecting spirometry accuracy
Spirometry accuracy can be influenced by several factors, including patient effort, technician skill, and equipment calibration. Suboptimal patient effort, improper technique, and equipment malfunctions can lead to inaccurate results. Ensuring proper training for both patients and healthcare providers, as well as regular calibration and maintenance of spirometry equipment, is essential to obtaining reliable measurements.
Certain populations, such as young children and the elderly, may face challenges in performing spirometry. Young children often struggle to understand and perform the required maneuvers, leading to unreliable results. Similarly, elderly patients may have comorbidities or physical limitations that affect their ability to complete the test accurately.
Addressing these challenges in clinical practice
To address the challenges associated with spirometry, comprehensive training programs for healthcare providers are necessary. These programs should focus on proper test administration, patient coaching, and interpretation of results. Additionally, patient education on the importance of spirometry and correct performance techniques can improve test reliability. In cases where spirometry is not feasible, utilizing alternative diagnostic tools and incorporating clinical judgment is crucial for effective asthma management (CCJM) (ERS Journals). For children, using animated incentives, that provide visual feedback, can make the test more engaging and easier to perform. Ensuring a child-friendly environment and involving parents or caregivers in the process can further improve the reliability of the results.

Potential future applications in asthma care
Looking ahead, the future of spirometry and asthma management may include even more sophisticated technologies and applications. Artificial intelligence (AI) and machine learning algorithms have the potential to analyze spirometry data alongside other health metrics to predict asthma exacerbations with greater accuracy. These predictive models can identify patterns and early warning signs that may not be evident through traditional analysis, enabling preemptive measures to prevent severe asthma attacks.
Moreover, advancements in biomarker research could lead to the development of spirometry devices capable of detecting specific biomarkers in exhaled breath. These biomarkers could provide additional insights into airway inflammation and other underlying physiological changes, offering a more comprehensive assessment of asthma control.
Personalized medicine is another promising area, where spirometry data could be used to tailor treatments based on individual genetic profiles and specific asthma phenotypes. This approach aims to optimize therapy by targeting the unique characteristics of each patient’s asthma, resulting in more effective and targeted interventions.
In summary, the future of spirometry and asthma management is bright, with ongoing technological advancements and innovations poised to revolutionize respiratory healthcare. By embracing these developments, healthcare providers can offer more accurate, accessible, and personalized care, ultimately improving outcomes for patients with asthma.
Conclusion
Spirometry is a cornerstone in the management of asthma, providing essential data for accurate diagnosis, monitoring, and treatment. Despite its challenges, the benefits of spirometry in improving asthma control and predicting exacerbations are undeniable. By incorporating spirometry into routine asthma care, healthcare providers can enhance patient outcomes and reduce the burden of asthma. Future advancements in technology and increased awareness of spirometry’s importance will likely further its role in asthma management, ensuring that patients receive the best possible care.
References
- “Treatment strategies for asthma: reshaping the concept of asthma management.” Allergy, Asthma & Clinical Immunology. Available at: aacijournal.biomedcentral.com
- “Managing adult asthma: The 2019 GINA guidelines.” Cleveland Clinic Journal of Medicine. Available at: ccjm.org
- “European Respiratory Society Guidelines for the Diagnosis of Asthma in Adults.” European Respiratory Society. Available at: erj.ersjournals.com
- “Asthma: Updated Diagnosis and Management Recommendations from GINA.” American Academy of Family Physicians. Available at: aafp.org
This article has been reviewed by
Elina Kiviaho
Senior Biomedical Laboratory Scientist, Clinical Expert in Biomedical Analytics
Linkedin