Asthma control: what patients need to know in 2025
Asthma is a condition that affects millions of people worldwide, yet it often goes misunderstood or underestimated. According to the Global Asthma Report 2024, over 340 million people are living with asthma, and the numbers continue to rise due to environmental factors and urbanisation. While some experience mild, occasional symptoms, others face daily challenges in managing their breathing, energy levels, and quality of life. The good news? Asthma control has never been more achievable than it is today. With better awareness, updated treatment options, and a proactive approach, 2025 brings new possibilities for patients to take control and breathe easier.
Understanding asthma means recognising that it is a chronic inflammatory condition of the airways. It causes episodes of wheezing, shortness of breath, chest tightness, and coughing. These symptoms can vary in intensity and frequency, often triggered by allergens, exercise, cold air, or stress. While there is no cure, modern treatments and monitoring allow many to live active, unrestricted lives.
The importance of personal asthma control
Every case of asthma is unique. What works for one person might not be suitable for another. That is why asthma control begins with understanding your own patterns and triggers. In 2025, personalised care is more accessible than ever. Healthcare providers encourage patients to take an active role – not only by following prescribed treatments but by tracking symptoms and recognising early warning signs.
Uncontrolled asthma can lead to flare-ups that may require emergency care and, over time, cause permanent changes to lung function. On the other hand, well-managed asthma reduces the risk of exacerbations and allows for full participation in daily life, work, and exercise.
Monitoring lung health: why it matters
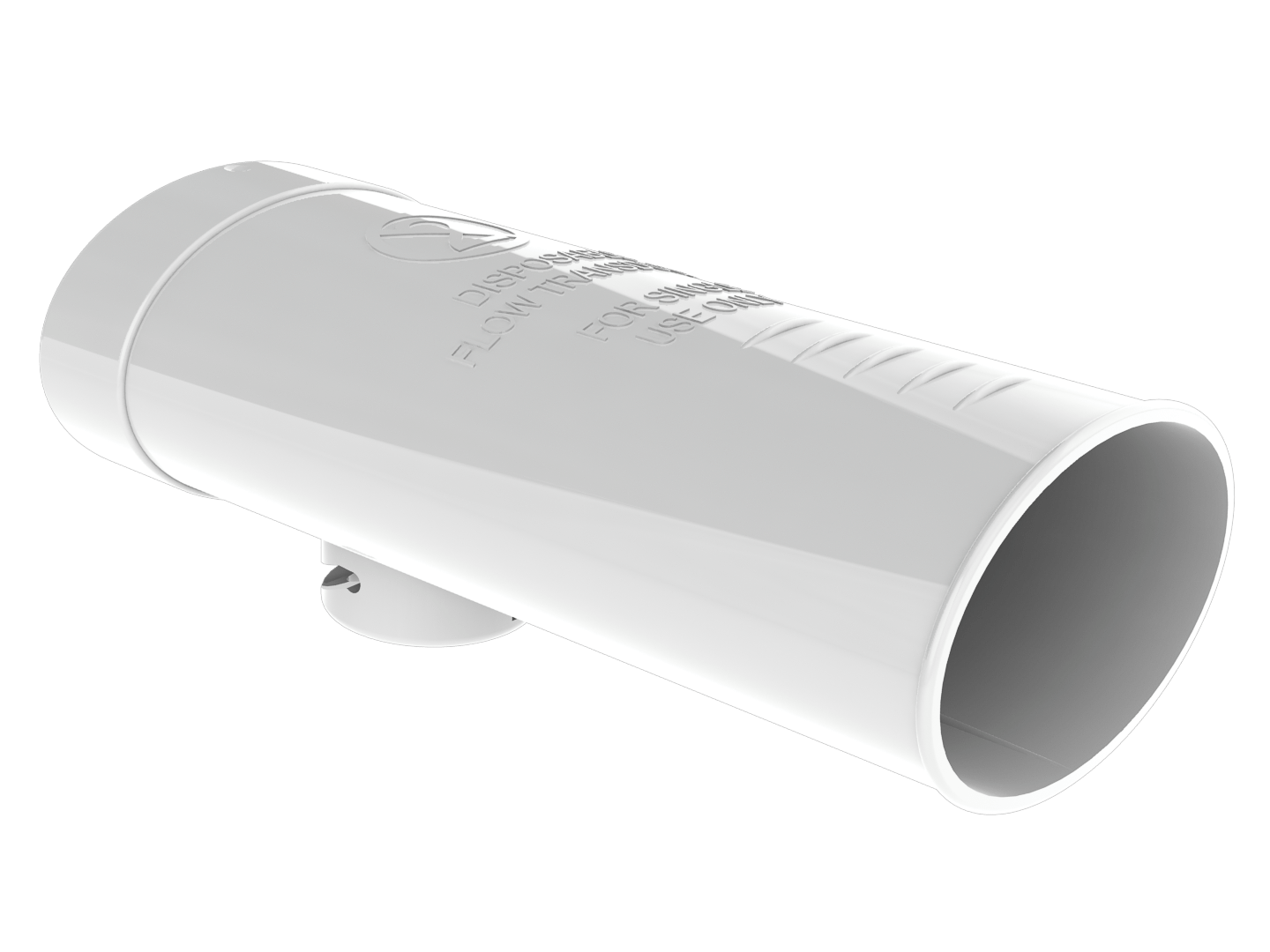
One of the key tools in asthma management is lung function monitoring. Spirometry, a simple and non-invasive test, measures how well your lungs are working. It helps detect changes even before symptoms become noticeable, allowing for early adjustments in treatment.
In 2025, spirometry is widely used not only in clinics but increasingly available in primary care and community settings. Initiatives across Europe, such as the “Breathe Better” programme, have expanded access to spirometry for at-risk populations, making it easier for patients to receive regular assessments. For patients, regular spirometry tests offer reassurance and insight. They provide tangible data that helps both the patient and healthcare provider understand whether the current treatment plan is effective.

Medication: what is new and what remains essential
The foundation of asthma treatment remains consistent – anti-inflammatory preventers (usually inhaled corticosteroids) and relievers (such as bronchodilators) used as needed. However, 2025 has brought refinements in how these medications are delivered and prescribed.
Smart inhalers, which track usage and remind patients when to take doses, are more commonly prescribed. A recent study in 2024 showed that patients using smart inhalers experienced a 30 % reduction in exacerbations compared to those using traditional inhalers. These devices also help healthcare professionals identify patterns of underuse or over-reliance on relievers. Combination therapies have also evolved, offering better symptom control with fewer side effects.
Importantly, patients are encouraged to understand their medication – knowing what each inhaler does, how to use it correctly, and when to adjust the approach based on symptoms. Pharmacists and nurses play a key role in this education, ensuring that every patient feels confident in their routine.

Lifestyle factors: beyond medication
While medication forms the cornerstone of asthma management, lifestyle also plays a significant role. Air quality, physical activity, nutrition, and stress management all influence asthma control.
- Air quality: Monitoring indoor air for allergens and using air purifiers can reduce exposure. Outdoor air pollution remains a concern, and patients are advised to check air quality indexes before prolonged outdoor activities.
- Exercise: Far from being off-limits, physical activity is encouraged. With good asthma control, most patients can participate fully in sports and exercise. Warming up, using preventive medication, and choosing suitable environments (e.g. avoiding cold, dry air) help ensure safe activity.
- Diet and weight management: Maintaining a healthy weight can reduce asthma severity. Certain diets rich in antioxidants and omega-3 fatty acids may also have supportive effects.
- Stress: Emotional stress can trigger asthma symptoms. Techniques such as breathing exercises, mindfulness, and regular routines help manage both stress and breathing patterns.
When to seek help
Knowing when to reach out to a healthcare provider is vital. If symptoms begin to interfere with sleep, work, or daily activities, or if reliever inhalers are needed more often than usual, it may be a sign that asthma is not well controlled. Early intervention can prevent exacerbations and restore balance.
In 2025, many clinics offer digital check-ins or remote consultations, making it easier for patients to access advice without delay. Keeping an asthma action plan – a written guide developed with a healthcare provider – helps patients know exactly what steps to take when symptoms change.

Looking ahead
Asthma management continues to improve, driven by both technology and a better understanding of the condition. In 2025, EU health policies have prioritised respiratory care, funding research and improving access to diagnostic tools across member states. Patients have more tools than ever to manage their health, from accurate diagnostics to personalised treatments and ongoing support.
Control is possible, and with awareness, regular monitoring, and collaboration with healthcare providers, patients can take an active role in shaping their own wellbeing. Breathing should not be a struggle – with the right approach, it becomes the quiet, reliable rhythm of a life fully lived.
This article has been reviewed by
Elina Kiviaho
Senior Biomedical Laboratory Scientist, Clinical Expert in Biomedical Analytics
Linkedin

More from the articles:
Cooperation that endures and evolves – Medikro and Savonia jointly build practice-oriented spirometry education
15.11.2025
Read moreCreating future professionals through collaboration – Medikro Spirometers in teaching at Oulu University of Applied Sciences
21.10.2025
Read more